Living with lupus
Amanda Stephenson • January 2, 2021
Invisible symptoms
Lupus is an autoimmune disease that causes your body's antibodies to attack it's own organs and tissues, triggering inflammation and pain. It is estimated that 1 in 1000 people in the UK have lupus. 90% of people with lupus are female, usually aged 15-45 with a greater prevalence in Black and Asian women. It takes on average 6.4 years to be diagnosed with lupus, often with other diagnoses suggested along the way.
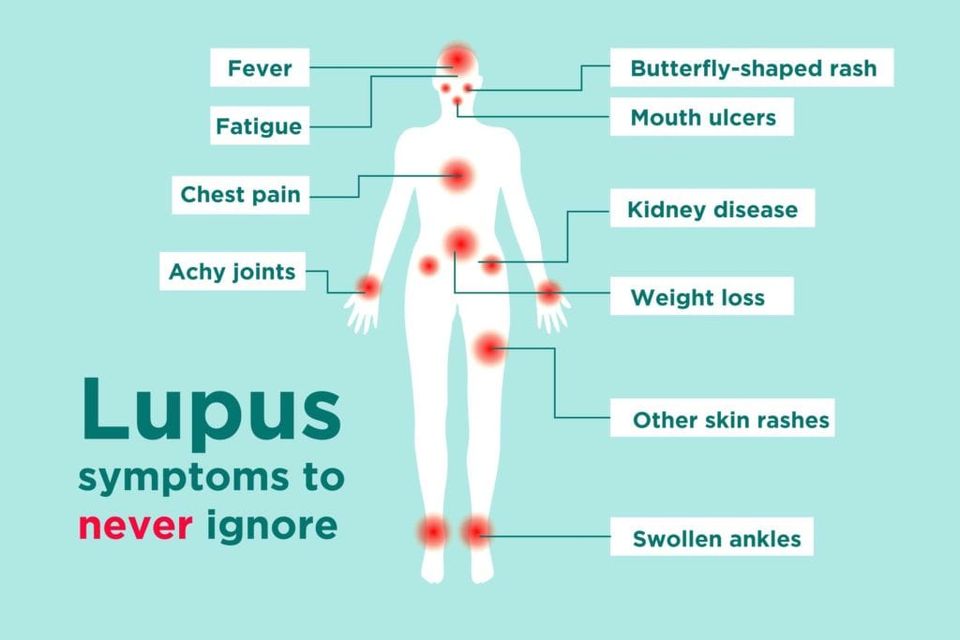
There are a large range of symptoms:
Skin rashes
Joint pain, stiffness or difficulty moving- especially in the morning and can take between minutes to hours to wear off
Joint swelling, warmth or tenderness to touch
Rashes from sunlight/UV light (including the classical "butterfly" rash on the cheeks and nose)hes from sunlight/UV light (including the classical "butterfly" rash on the cheeks and nose)
Flu like symptoms and or night sweats
Headaches, migraines
Fatigue (80-90% of people with lupus report this is their main symptom) - tiredness so severe it makes daily activities difficult
Brain fog
Dry eyes or mouth - sensation of sand in the eyes, regularly waking at night to drink water
Mouth or nasal ulcers - shallow or recurring ulcers or sores that won't heal
Unexplained weight gain or weight loss
Inflammation of the tissues covering internal organs with associated chest and/or abdominal pain
Seizures, mental illness or other cerebral problems
Kidney problems
Depression
Hair loss
Haematological disorders including anaemia
Swollen glands
Poor blood circulation causing the tips of fingers and toes to turn white then blue on exposure to cold (Raynauds)
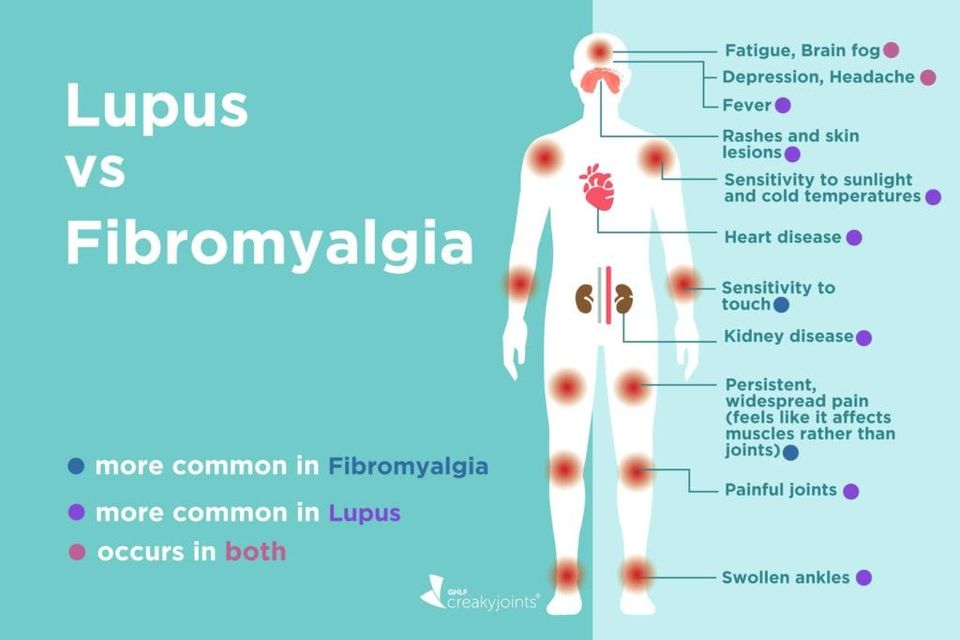
Many of these symptoms can become worse if you are stressed. People are often diagnosed with anaemia, eczema, fibromyalgia. We recommend that you tell your GP about your symptoms and keep a log of your symptoms, note their frequency and severity. You should be referred to an autoimmune / rheumatology specialist
Research is still trying to find what causes lupus - as it's mostly women that are affected it is thought there is a link with female hormone changes - progesterone and oestrogen - during puberty, pregnancy and menopause. Viral infections, long courses of some medications and trauma can trigger lupus. Sunlight can cause a flare up of lupus which may indicate an environmental link. Lupus is often triggered in people where there is family history of lupus and/or other immune system illnesses such as arthritis, MS and rheumatism. Most recently autoimmune conditions have been linked to our bodies gut bacteria, the microbiome. Black and Asian women may be more at risk of developing severe lupus due to healthcare inequalities.
Whilst there currently is not a cure for lupus, there are several things you can do to help manage the condition
from various sources including https://www.lupusuk.org.uk/manage-your-lupus/
Eat a Mediterranean diet ( no not pasta and pizza!), unprocessed food, lean meats, fish, olive oil, broad range of vegetables and fruit
Limit your alcohol intake
Try gentle exercise such as yoga
Join a support group for people with lupus
Become well-educated about lupus
Offset fatigue by rest and by pacing daily activities
Try to resolve stress, depression, pain or anger
Avoid exposure to direct sunlight and fluorescent lights
Be open with family and friends on lupus unpredictability
Develop new interests and skills if wished and if able
Ask for help from family, friends and health professionals
Lupus UK report that "Careful monitoring of the disease and a treatment programme with medication adjusted as appropriate enables the condition to be controlled, most patients being able to live a normal life span. Doctors will usually only keep the patient on high impact medication for as short a period as possible.
Non-steroidals, Aspirin etc - anti-inflammatory drugs (NSAIDS), used for patients who suffer mainly from joint/muscle pain. Aspirin, heparin or warfarin may be prescribed in the case of patients needing anticoagulation treatment.
Living with Pain
Anti-Malarials - these are of help in patients with skin and joint involvement and of some assistance with fatigue. The drugs may be sufficient for patients with moderately active lupus to avoid using steroids. Hydroxychloroquine has anti-inflammatory properties, some sun-protective features and gives some protection against clotting - mepacrine is also used.
Steroids such as prednisolone have been vital in the improvement in lupus care and in some cases are life saving. They have a profound effect on inflammation and suppress active disease. The dosage depends on the severity of the symptoms. Once the disease is under control the dosage might be reduced gradually and/or it might be possible for the patient to transfer to other medication. The side-effects of steroids are well-known and include possible weight gain, muscle weakness, and over time the possibility of osteoporosis. For more information go to:
Medicine Guide for steroids
Immunosuppressants - these drugs are widely used in more severe disease. The most commonly used are azathioprine, methotrexate and cyclophosphamide. Azathioprine is a milder drug and used for mild to moderate kidney disease, or where its difficult to reduce steroid dosage. Cyclophosphamide, usually given by pulse, is widely used for kidney disease and is very effective. Regular blood testing is required initially 2-3 weekly, subsequently 4-6 weekly whilst on such medication. For more information on these drugs go to:
Other drugs - Other drugs are less frequently used in lupus and include intravenous immunoglobulin (often used when the platelets are low) and cyclosporin A, the drug widely used in transplantation medicine to suppress rejection. For very severe skin disease in patients where pregnancy is not a consideration, thalidomide has proved an extremely powerful medication.
Non-lupus drugs - Various medications have helped improve the prognosis in lupus. These include a variety of improved blood pressure tablets and diuretics, anticoagulants (aspirin or warfarin) in those patients with a clotting tendency, anti-epileptic and anti-depressive medication. Skin creams include corticosteroids and newer, vastly improved sun-protection creams. There are now, in addition to standard calcium and vitamin D preparations, modern effective drugs for the prevention and treatment of osteoporosis."
"Exercise is an important part of taking care of yourself and your wellbeing. Just like everyone else, where possible, people with lupus need to exercise regularly or engage in some kind of movement. It’s very important to recognise that lupus affects everybody differently and so not everyone with lupus can do a wide range of exercises, but most people with lupus can take part in some form of activity. It is also important to realise that the amount of activity you can manage is likely to fluctuate as your lupus does." It is recommended that you check with your GP or autoimmune consultant which exercise is suitable for you.

In recent years there has been increasing research into the digestive tract and the many ways in which it interacts with our body and brain. To have good gut health means that your gastrointestinial tract (oesophagus, stomach and intestines) is in the best possible. condition. This involves the gut microbiome - the microbes- a mixture of bacteria, viruses and fungi that live in our digestive system. They are important for good health and disease prevention and the higher level of good microbes (probiotics) in our biome the better. What are the symptoms of poor gut health? If your gut health is not optimal you may experience abdominal pain, discomfort, constipation, diarrhoea, heartburn or indigestion. Even if you have no symptoms it remains important to look after your gut as increasingly scientists are finding that gut health is a major factor in our immunity. Good gut health can also protect against type 2 diabetes, bowel cancer and heart disease. Poor gut health can also have an effect on mood and mental wellbeing- due to the gut-brain axis. This is a two way communication network between the brain and the gut, linked by nerves, hormones and neurotransmitters acting as chemical messengers. How can I improve my gut health? Increase your fibre intake - we should consume 30g of fibre a day Most people only manage about 18g of fibre a day. Eating a combination of soluble and insoluble fibre adds bulk and improves the transit time of food through the digestive system. Gut bacteria loves fibre, but it is recommended to increase your fibre intake gradually to avoid bloating. By eating a variety of fruit, vegetable, pulses, wholegrains and nuts your gut health will improve. Sources of soluble fibre - oats, linseeds/flaxseeds, lentils, fruit and vegetables. Sources of insoluble fibre - nuts, wholewheat flour, wholemeal bread, wheat bran, beans,cauliflower, green beans and potatoes Seven great foods for your microbiome Apples are high in pectin a prebiotic - one apple contains 4g of fibre Oats are high in a dietary fibre called beta-glucan which can help lower LDL cholesterol if eaten regularly Onions are a good source of prebiotics Kefir is rich in probiotic bacteria and calcium. It can help restore your gut after you have taken antibiotics which can reduce good gut bacteria Wholegrain carbohydrates such as w hol emeal bread and pasta and brown rice can easily increase your fibre Lentils are full of soluble fibre which helps food transit through the digestive system Fermented foods such as sauerkraut kimchi may improve intestinal health and as a result support the immune system and anti-inflammatory responses and improve levels of good bacteria in the gut. Drinking plenty of fluids is great for gut health. 6-8 200ml glasses of water a day is recommended. Professor Tim Spector, specialist in genetic epidemiology, writes in his book Spoon-Fed how artificial sweeteners and processed foods are bad for our gut health. He advises avoiding anything labelled as a “diet” food and especially anything containing artificial sweeteners which, he suggests, can trick our bodies into gaining weight. Regular exercise 30 minutes of moderate activity ( moderate = going for a walk at a good pace but still being able to chat) five times a week helps regulate bowel movements and can help boost gut bacteria. Calcium can boost the production of digestive enzymes which break down proteins, carbs and fats and helps the absorption of nutrients - so a small 30g snack of cheese, 120g yogurt or kefir for breakfast or 200ml of milk will help. Should I take prebiotics and probiotics? Prebiotics are non-digestible food compounds like fibre that feed the good bacteria and help digestion and nutrient absorption. You do not need to buy them in a pill - you can get them from wholegrains and fruit and vegetables such as asparagus, Jerusalem artichokes, onions, garlic and under-ripe bananas. Probiotics are the good bacteria themselves such as Lactobacillus and Bifidobacterium species. If your yogurt is live they will be listed in the ingredients list. They are also found in fermented foods such as kimchi, kombucha, tempeh, kefir and sauerkraut (not all sauerkraut has live bacteria as some brands are pasteurised). To boost gut bacteria we should eat both prebiotics and probiotics, whilst avoiding highly processed foods. Professor Tim Spector advises avoiding any food that comes in a packet with more than 10 ingredients listed.

Menopause was a word that was usually whispered and given all manner of euphemisms from "it's my age" to " personal moment" and " hot flush". Women often struggled through it and men tended to toddle off the pub or the shed or quite frankly anywhere to get away from it. Times are changing. In 2015 the then Chief Medical Officer Professor Dame Sally Davies stated that " Menopause should be discussed as openly as any other subject". Young people now learn about it in secondary school, which makes sense as their Mum's will go through it and half of them will experience it in later years. There still remain some hurdles to discussing menopause - explaining symptoms to work colleagues or managers is difficult. Asking for 10 mins outside to cool down is no different to people racing outside for their cigarette break or their Starbucks fix. As with many things in life forewarned is forearmed - if you know about the symptoms and what can happen you will feel better prepared to manage it. What is perimenopause? Usually it happens between the age of 45-55. For 1 in 100 women it will start under the age of 40. Perimenopause means "around menopause" and refers to the time during which your body makes the natural transition to menopause, marking the end of the reproductive years. Perimenopause is also called the menopausal transition. Women start perimenopause at different ages. You may notice signs of progression toward menopause, such as menstrual irregularity, sometime in your 40s, some women notice changes as early as their mid-30s. The level of estrogen — the main female hormone — in your body rises and falls unevenly during perimenopause. Your menstrual cycles may lengthen or shorten, and you may begin having menstrual cycles in which your ovaries don't release an egg (ovulate). You may also experience menopause-like symptoms, such as hot flushes, sleep problems and vaginal dryness. Your GP can discuss the treatments which are available to help ease these symptoms. Once you've gone through 12 consecutive months without a menstrual period, you've officially reached menopause, and the perimenopause period is over. Perimenopause symptoms Irregular periods As ovulation becomes more unpredictable, the length of time between periods may be longer or shorter, your flow may be light to heavy, and you may skip some periods. If you have a persistent change of seven days or more in the length of your menstrual cycle, you may be in early perimenopause. If you have a space of 60 days or more between periods, you're likely in late perimenopause. Hot flashes and sleep problems Hot flushes are common during perimenopause. The intensity, length and frequency vary. Sleep problems are often due to hot flashes or night sweats, but sometimes sleep becomes unpredictable even without them. Mood changes Mood swings, irritability or increased risk of depression may happen during perimenopause. The cause of these symptoms may be sleep disruption associated with hot flashes. Mood changes may also be caused by factors not related to the hormonal changes of perimenopause. Vaginal and bladder problems When estrogen levels diminish, your vaginal tissues may lose lubrication and elasticity, making intercourse painful. Low estrogen may also leave you more vulnerable to urinary or vaginal infections. Loss of tissue tone may contribute to urinary incontinence. Decreasing fertility As ovulation becomes irregular, your ability to conceive decreases. However, as long as you're having periods, pregnancy is still possible. If you wish to avoid pregnancy, use birth control until you've had no periods for 12 months. Changes in sexual function During perimenopause, sexual arousal and desire may change. If you had satisfactory sexual intimacy before menopause, this will likely continue through perimenopause and beyond. Loss of bone mass With declining estrogen levels, you start to lose bone more quickly than you replace it, increasing your risk of osteoporosis — a disease that causes fragile bones. Changing cholesterol levels Declining estrogen levels may lead to unfavorable changes in your blood cholesterol levels, including an increase in low-density lipoprotein (LDL) cholesterol — the "bad" cholesterol — which contributes to an increased risk of heart disease. At the same time, high-density lipoprotein (HDL) cholesterol — the "good" cholesterol — decreases in many women as they age, which also increases the risk of heart disease. Problems with memory or concentration Risk factors Menopause is a normal phase in life which may occur earlier in some women than in others. Although not always conclusive, some evidence suggests that certain factors may make it more likely that you start perimenopause at an earlier age, including: Smoking. The onset of menopause occurs one to two years earlier in women who smoke than in women who don't smoke. Family history. Women with a family history of early menopause may experience early menopause themselves. Cancer treatment. Treatment for cancer with chemotherapy or pelvic radiation therapy has been linked to early menopause. Hysterectomy. A hysterectomy that removes your uterus, but not your ovaries, usually doesn't cause menopause. Although you no longer have periods, your ovaries still produce estrogen. But such surgery may cause menopause to occur earlier than average. Also, if you have one ovary removed, the remaining ovary might stop working sooner than expected. Complications Irregular periods are a hallmark of perimenopause. Most of the time this is normal and nothing to be concerned about. However, see your doctor if: Bleeding is extremely heavy — you're changing tampons or pads every hour or two for two or more hours Bleeding lasts longer than seven days Bleeding occurs between periods Periods regularly occur less than 21 days apart Signs such as these may mean there's a problem with your reproductive system that requires diagnosis and treatment. How will I feel during perimenopause? Approximately 75% of women experience hot flushes, sweats, tiredness, poor concentration, memory deficits, brain fog or vaginal and bladder problems. But do not worry - they do not tend to happen all at once! Some symptoms will be more prevalent than others and will settle, go away and can return later on.Most women find that symptoms go away completely and some women hardy have any symptoms at all. There are also dietary and lifestyle changes that can help improve symptoms and the GP can discuss these and hormone replacement therapy with you. It is very common to feel tearful due to the fluctuation of hormones, the stress of dealing with the symptoms alongside work and daily life. It is also common to feel anxious or depressed. Using mindfulness and breathing techniques can help ease anxiety but if you or those around you suspect worsening anxiety or depression then you should discuss this with your GP. Can changing what I eat help? Perimenopause can cause weight changes including weight gain. Reducing sugar and saturated fats, changing to complex carbohydrates such as wholegrains will make a difference. Adding plant oestrogens such as flax seed, rye and soy products may reduce your hot flushes a little. Eating a calcium rich diet (dairy, nuts, non-dairy alternative or spinach) can improve your bone health and ensuring you have sufficient Vitamin D ( oily fish – such as salmon, sardines, mackerel, trout. red meat, l iver and fish liver oil, egg yolks) especially in winter months when we cannot get out in the sunshine, will all help. How can I keep healthy? Good health throughout the menopause is important for your future health. Not smoking, eating a balanced diet, maintaining a healthy weight, limiting alcohol and doing regular weight bearing and resistance exercise will build the foundation blocks for good heart and bone health ( see my blog on osteopenia and osteoporosis). Stress reduction is also important so factor in regular time for relaxation and exercise. Where can I get more information? Led by specialist gynaecologist Dr Heather Currie www.menopausematters.co.uk is an excellent source of information The British Menopause Society has information on women's health www.womens-health-concern.org and a list of menopause specialists searchable by postcode www.thebms.org.uk For employers who want to support women through this life transition https://peppy.health/menopause/ Menopause : The One Stop Guide Kathy Abernethy, menopause specialist nurse www.kathyabernethy.com What is post-menopausal? Once your periods have stopped for a year, you are considered post menopausal. Menopausal symptoms can last around 4 years after your last period, although some women experience them for much longer.

1. Do not avoid lifting heavy things By avoiding lifting heavy items people are actually doing their back more harm, not putting sufficient load through the muscles causes deconditioning and stiffness. Fiona Wilson, associate professor of physiotherapy says "the back needs to be exposed to loads to become stronger. Proceed gradually, especially if you haven’t lifted anything heavy for a while. In studies on elite rowers, who load their l ower backs significantly in training, Wilson has shown that those who increase their training loads too rapidly are more likely to get back pain. Start lifting things such as shopping and books as part of your daily routine, and don’t be afraid to add weights as you get stronger,” she says. “Get used to carrying different loads in different ways.” 2. Don't avoid bending and twisting The spine is designed to bend and twist - that's why it is a curve! Wilson says " It’s not always best to bend from the hips, keeping your back straight. This advice is to encourage the use of the muscles in the hips and legs to help with the bending,” Wilson says. “But if those muscles are weak, it won’t protect your back and, in fact, the spine is a more stable structure when it is curved.” Bending and twisting in a variety of ways within your comfort zone is the best approach. 3. Try this exercise - the prone windmill Matt Roberts, a personal trainer, speaking in The Times says this simple exercise is great for engaging the upper back muscles and encouraging twisting of the back. Start on all fours on the floor and raise your left arm towards the ceiling. Turn your head to look at the straight arm as you raise it. Lower the arm and perform a big rotation to take it underneath your torso as far as is comfortable. Repeat this for 15-20 rotations before switching to the right arm.
The charity Versus Arthritis surveyed 1040 remote workers. More than four out of five people who began home working during lockdown have experienced musculoskeletal pain - that is back pain, shoulder pain and neck pain. They found that 89% of staff had developed these conditions but had not mentioned it to their employer. Understandably people were reticent about complaining due to the ever increasing numbers of people being made redundant and faced with a new way of working many people did not know their rights when working from home. Remote flexible working can be easier to fit around childcare and offer opportunities to work for people with impairments and health conditions. However many people have worked longer hours in unsuitable conditions - up to 45% of staff did not receive equipment, advice or support from their employer for homeworking. 23% of staff said they experienced pain most or all of the time and 46% of staff had been taking pain relief more frequently than usual. Over 50% of staff reported low back pain, 36% reported neck pain and 28% had experienced shoulder pain, only a third of staff had spoken to a medical or health professional during lockdown about their musculoskeletal pain. If you have musculoskeletal pain it is important to seek medical or healthcare professional advice early to help resolve the symptoms and avoid taking time off work. It also reduces the risk of needing more invasive treatment when the condition has become a long term complaint. One of the simplest things you can do when working from home is to get up from your kitchen/dining table/desk/sofa every 30 mins and have a walk about. Take your cuppa outside ( if the weather allows!) Musculoskeletal problems tend to develop from staying in one position for too long rather than sitting on the wrong sort of chair. Ergonomic desks/standing desks/ specialist equipment are generally very expensive and current research shows they may not be very effective at reducing shoulder, back or neck strain. Taking steps to lower your stress levels can also reduce the likelihood of musculoskeletal pain - taking regular exercise, enjoying a warm bath, taking the dog for a walk or watching a comedy can all help. If you are experiencing musculoskeletal pain Physio In The Sticks can help. We are available for home visits or online consultations 7 days a week www.physiointhesticks.co.uk 07398 495819. We frequently resolve musculoskeletal conditions in 1-3 appointments.

The knock on effects of bed rest are known as deconditioning syndrome and are one of the most under recognised and unreported side effects of a hospital stay. It is estimated that older hospital patients may spend up to 95% of their time in bed or sitting in a chair. Whilst recently editing this year's medical school resources I learnt some concerning facts. Patients going into hospital.... with high mobility (that is you can walk about well and do all your daily activities) average 13% disabled at discharge go in with moderate mobility (walking about with a stick, able to do some daily activities) average 35% disabled at discharge go in with low mobility (walking about with a stick, usually rely on others to do most daily activities) average 71% disabled on discharge 65% patients over 90 years old lose the ability to do their daily activities this functional decline is seen as early as day 2 of a hospital stay Contrary to popular belief, bed rest is not a good way to recover from many illnesses and it can hinder recovery time, especially as it makes patients more susceptible to muscle wasting, weakness, pressure ulcers, poor digestion, constipation, loss of appetite, tiredness, lethargy, low mood and confusion. Yes there are risks to moving about, especially if you have low/high blood pressure, previous history of falls, muscle weakness or joint pain but the risk of remaining inactive is usually higher. With a just few physio sessions, we can help people regain their muscle strength, improve their balance and return to previous levels of independence. Physio In The Sticks offer home visits at a time to suit you. If you would like help for yourself or a relative please call Amanda 07398 495819 info@physiointhesticks.co.uk

Following the stop-start nature of lockdowns and a new interest in keeping healthy for many - the home workout may be here to stay long term. There are advantages to a home workout - no membership fees, no travelling to a gym and easier to fit in a quick 10 minutes of exercise. A few key pieces of equipment can help you get the most out of your time. Resistance bands - these are very effective for back and shoulder exercises that involve pulling. They often can be bought in a budget-friendly set of three strengths - start with the easiest band and gradually increase to the harder band over several months. Dumbbells -a single set of dumbbells can work nearly every muscle in your body. You can start with a couple of tins of baked beans or small bottles of water can be easier to grip. Different people can manage different weights but as a general rule any weight you can raise above your head confidently 5 times is ideal. Dumbbells can bought for £10-£25 for a basic set of 2-6kg. Kettlebells - are great for functional resistance - which is basically means exercise which replicates your daily activity, such as carrying shopping and lifting heavy items. You can start with a rucksack with a few tins of beans inside. They are useful for one sided exercises to help you build strength on both sides of your body. They start at 4kg Yoga mat - a non-slip mat with good cushioning is the best option. Good underside grip will prevent you from sliding when doing lunges and people with wrist or knee pain will appreciate a mat with a thickness of 6mm or more. TRX band is a total body resistance band with handles which lets you use your body weight and gravity as resistance to build strength, balance, coordination, flexibility and joint stability. The TRX can replicate some of the exercises done on gym machines by looping it around a sturdy tree trunk or stair post.

In the UK over 3 million people have osteoporosis. Over 500,000 have hospital treatment for fragility fractures related to osteoporosis. Our genes determine our height and skeleton type but our bone health is related to our lifestyle choices over many years. Reduction in bone mass is a normal part of the ageing process - but it does not have to be. Women are at greater risk than men. The reduction of oestrogen following menopause causes women to lose bone mass more quickly for the few years after menopause. Women who experience early menopause (before 45 years of age) or who have had their ovaries removed are at greater risk. Younger women, children and men may still have osteoporosis. In the UK over 1/3 women and 1/5 men will have a fragility fracture in their lifetime and at age 75-84 the 10 year risk for having a fragility fracture is 24% women and 14% men. Osteopenia is the stage of bone thinning before osteoporosis. Osteopenia does not necessarily lead to osteoporosis and your doctor may prescribe bone strengthening treatments to prevent further bone loss. Osteoporosis is a combination of bone mass and bone quality reduction. As bones weaken the risk of fracture increases. The first time people may suspect osteoporosis is following a pain caused by a bone fracture, which can be the result of a low impact injury. Fractures to the wrist, neck of femur (part of the thigh bone that forms the hip joint) and spine (vertebrae) are common. Ribs, pelvic bones and arms are also seen frequently. Older adults may have a forward bent over or stooped posture that can indicate fractures of the spine (vertebrae). There are many factors that increase the risk of osteoporosis: 1. taking high-dose steroid tablets for more than 3 months 2 medical conditions – such as inflammatory conditions, such as rheumatoid arthritis, or malabsorption problem such as coeliac disease 3. family history of osteoporosis – particularly a hip fracture in a parent 4. long-term use of certain medicines that can affect bone strength or hormone levels, such as anti-oestrogen tablets that many women take after breast cancer 5. having or having had an eating disorder such as anorexia or bulimia 6. having a low body mass index (BMI) 7. not exercising regularly 8 heavy drinking 9. smoking 10. absent periods for 6 months or more caused by over exercising or over dieting 11. low testosterone levels in men 12. overactive thyroid gland 13. disorders of the adrenal glands, such as Cushing's syndrome 14. disorders of the pituitary gland 15. overactivity of the parathyroid glands 16. long periods of inactivity or bed rest You can find out if you are at risk of osteoporosis by doing the Royal Osteoporosis Society's online test https://stopatone.theros.org.uk/ How to help your bones stay healthy Diet - ensure you have plenty of.... 1. Calcium found in milk, cheese and other dairy foods, green leafy vegetables – such as curly kale, okra and spinach, soya drinks with added calcium, bread and anything made with fortified flour, f ish where you eat the bones – such as sardines and pilchards 2. Vitamin D From about late March/early April to the end of September, most people should be able to get all the vitamin D they need from sunlight. The body creates vitamin D from direct sunlight on the skin when outdoors. However, between October and early March we do not get enough vitamin D from sunlight. Vitamin D is also found in a small number of foods including oily fish – such as salmon, sardines, herring and mackerel, red meat, liver, egg yolks, f ortified foods – such as some fat spreads and breakfast cereals. Another source of vitamin D is dietary supplements. Exercise The Royal Osteoporosis Society say that after a diagnosis of osteoporosis or if you have risk factors, you should do more exercise, rather than less. Being physically active and exercising helps you in so many ways, and is very unlikely to cause a broken bone. If you have spinal fractures or lots of other broken bones, you may need to modify some exercises to be on the safe side.There are three ways that exercise and safe movement help with bone health and osteoporosis: Promote bone and muscle strength Keep you steady Care for your back What types of exercise do I need to do for my bones? Bones stay strong if you give them work to do. For exercise to be most effective at keeping bones strong you need to combine weight-bearing exercise with impact and muscle strengthening exercise. Variety is good for bones, which you can achieve with different movements, directions and speeds - in an activity like dancing for example. Short bursts of activity may be best, such as running followed by a jog, or jogging followed by a walk. What is weight-bearing exercise with ‘impact’? You are weight bearing when you are standing, with the weight of your whole body pulling down on your skeleton. Weight bearing exercise with impact involves being on your feet and adding an additional force or jolt through your skeleton – anything from walking to star jumps. You can get weight bearing exercise with impact by taking part in some physical activity, sports or by doing specific exercises. Depending on what activity you do, the level of impact will vary. The following will help you to understand the difference between low, moderate and high impact exercise: Low impact Walks, Brisk walking Marching Stair climbing Gentle heel drops Stamping Moderate impact Highland dancing Jogging or running Team & racket sports Skipping & hopping Low level jumping Stamping High Impact Basketball Volleyball Track events Star jumps Tuck jumps High level jumps More physical activity information from the Royal Society of Osteoporosis can be found on their website www.theros.org.uk

In your 40's levels of the growth hormone somatotropin begins to decline. Somatotropin stimulates fat metabolism (the storage and breakdown of fat), cell reproduction, regeneration and growth. This can lead to increased fat storage, reduced muscle mass, lower libido and energy levels ( oh joy!) In addition as perimenopause approaches levels of oestrogen and progesterone decline. When oestrogen declines fat lays down around your belly instead of on your hips and thighs. As we know belly fat is more concerning for increasing the risk of diseases such as Alzheimer's, stroke, heart disease, colorectal and breast cancer and Type 2 diabetes. As muscle mass decreases and potentially activity lessens your metabolism starts to slow down which may cause weight gain. This tends to coincide with having the least amount of free time due to work and childcare responsibilities. However to lose weight does not mean endless hours on a treadmill. Increasing lean muscle mass with functional strength training is a great way to improve your fitness with limited time. Any functional movements that you do in your usual day such as pushing, pulling, walking, lifting, bending can increase muscle mass and even more so if you add some ankle or wrist weights or a back pack with a couple of bags of sugar/flour. High Intensity Interval Training HIIT is also a great way to fit in effective exercise that works multiple muscle groups at once and includes cardio work and it can take as little as 8 minutes. 3 sessions of HIIT a week plus 2 x 30 minutes sessions of strength training and you will feel ready for anything! Remember to include 2 rest days a week as recovery is as important as exercise. Swimming (when we can!) is a great exercise which uses a wide range of joint movements and improves cardiovascular fitness if done fast enough. In your 50's - As we get older we may compare our abilities with how our bodes used to be - but really we should compare ourselves to yesterday not 10 years before! Due to added stress on ligaments and joints the key aim should be to maintain steady consistent training, rather than a sudden high impact exercise. It may help to track your activity to ensure a consistent level of exercise. Low impact exercise such as pilates, yoga, cycling and swimming are a good addition to walking, running, gardening and strength sessions. The average age a UK woman experiences the menopause is 51. Your body stops producing oestrogen which most people know is very important for bone health but what is not so well known is it's role in protecting heart health. Therefore in our 50's it's key to maintain a healthy heart with regular cardiovascular exercise and keeping within a healthy weight range. As muscle mass declines 32% of women in their fifties experience pelvic floor disorders such as urge incontinence, when urine leaks as you feel a sudden, intense urge to pee, or soon afterwards or overflow incontinence (chronic urinary retention) – when you're unable to fully empty your bladder, which causes frequent leaking. This can be exacerbated by drinking too much caffeine (coffee, tea, cola), sweeteners (in drinks, diet foods) and acidic fruit juices (orange, grapefruit). Contrary to the multitude of incontinence product adverts on TV - it is not a problem you have to tolerate. A few sessions with a pelvic health/women's health physio who can give you some simple exercises to do at home such as pelvic floor exercises, dead bugs, bridging and bird dogs - should help resolve the problem. I have heard many women's pelvic health physios recommend the book Me & My Menopausal Vagina by Jane Lewis and the Pelvic Obstetric and Gynaecological Physiotherapy group have information at https://pogp.csp.org.uk/information-patients Pilates is an excellent strength training exercise for women in their 50's, combining bodyweight resistance training, balance and flexibility. Using resistance bands and free weights for strength training exercises and weight bearing exercises such as running, zumba, tennis or netball are all great options for maintaining good bone health and muscle mass In your 60's It's important to keep doing the same exercises as before but with adjustments that allow for how our bodies are changing. In this decade your cartilage thins and the "grease" for your joints, synovial fluid decreases. The hydration and elasticity of ligaments reduces which in combination may mean that you start to feel achy joints more. If you happen to have an MRI or xray of your joints do not be alarmed by the word "degeneration" - much like grey hair or wrinkles we can manage these signs of ageing. Exercise promotes the circulation of synovial fluid and brings nutrients, oxygen and blood to the joints - motion is lotion! Exercise also increases muscle mass which decreases the load on the joints. Bodyweight resistance exercise with balance exercises which load your joints evenly is excellent at this age - so Pilates fits this perfectly. Tai chi and yoga are also great for mobility, flexibility and balance. Exercises which can be done easily at home with a sturdy chair such as calf raises, single leg balances and sit to stand are effective and can be found on the Chartered Society of Physiotherapy website www.csp.org.uk/publications/never-too-late-physiotherapy-advice-maintaining-strength-we-age Whilst this may be the age that many women retire, it is important to maintain activity levels. A decent daily walk is a great, free exercise - people with low step counts were found to have greater issues with mobility and balance in their later years. Walking a few steps around the home may add up but it does not give the benefits of stride length and hip and shoulder girdle mobility of a brisk walk outside. Investing in some decent walking shoes/boots can make walking more comfortable than in wellies! If you don't like walking alone, a quick search on Google will find a walking group near you.